BY DR EDGAR TAY, CARDIOLOGIST, INTERVENTIONAL CARDIOLOGIST
In 1998, a high school trumpeter experienced repeated episodes of numbness of his face after practice and subsequently could not use his left arm and leg due to weakness for several hours.
The action of forceful blowing against resistance is also known as the Valsalva Maneuver named after the 18th Century Italian anatomist who described the muscles involved with this action.
It is not just blowing a brass instrument but other actions such as weight lifting or even heavy straining while doing one’s business in the loo requires the use of such a manoeuvre.
So how does a stroke occur? This may be associated with a cardiac condition called a patent foramen ovale.
Let’s take a look at the heart structure in a bit more detail.
We all had a hole in our heart called the foramen ovale when we were still in our mother’s womb. This hole enables nutrient rich blood from the mother to passage from our right heart to the left chambers. This ‘hole’ closes after birth in most people. In a quarter of us this ‘hole’ remains open – we call this a patent foramen ovale or PFO
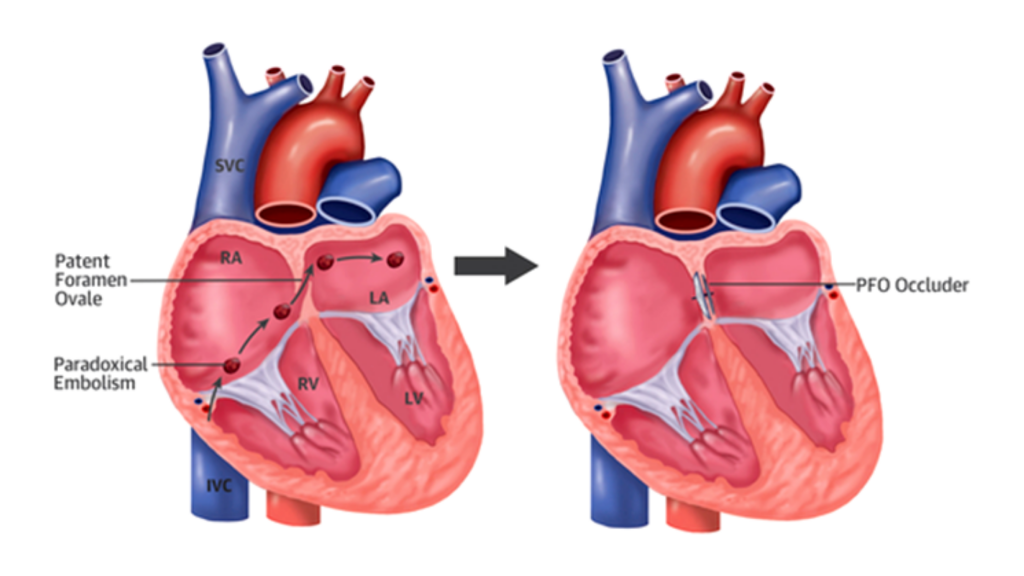
There are physiological changes that take place when doing the valsalva manoeuvre. Firstly, a dramatic increase in the pressure within the chest leads to reduced blood flow returning to the left heart. Left heart pressures fall. This results in a relative higher right heart chamber pressure resulting in right to left flow across the PFO.
The perfect storm.
Sometimes, tiny blood clots may develop in our veins. These clots migrate to the right heart and are usually filtered by our lung before returning to the rest of the circulation. When a PFO is present and the valsalva manoeuvre is performed, this clot can bypass the lung filtration and traverse directly through the PFO to the left heart, which then pumps this clot to the brain. This clot obstructs blood flow suddenly resulting in stroke. This is the outcome when all three events occur at that moment.
Can we prevent such event from occurring?
The strategy is multi-pronged.
1. Prevent blood clots from forming. Staying well hydrated and avoid sedentary work or sitting for long periods.
2. Be aware of stroke like symptoms. When these occur, consult your neurologist. Sometimes medications may be needed to reduce the risk of clotting.
3. In appropriate cases, assessment for a PFO may be needed. This entails ultrasound scans to demonstrate the presence of the PFO and consideration for a percutaneous procedure to close this defect may be needed. This would be done by a cardiologist.
In the case of this young patient, he was found to have a PFO and tests demonstrated that right to left shunting occured when he played the trumpet. The PFO was closed and these symptoms never recurred.
Learn more on the procedure of PFO here.

